
views
Recognizing Gallstone Symptoms
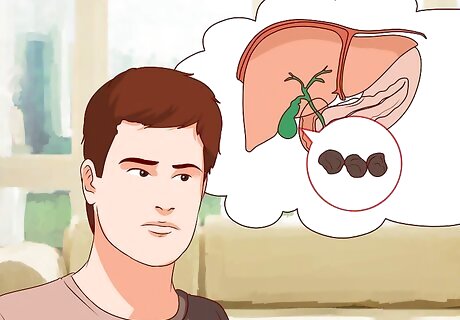
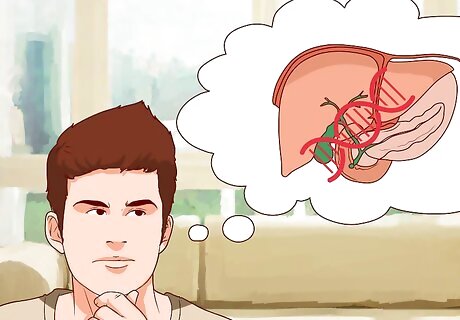
Be aware that gallstones are often asymptomatic. Gallstones can exist without ill effects for decades. Most people experience no symptoms when they have gallstones; in fact only 5 to 10% of people develop some symptoms of gallstones. This can make it difficult to know what to look for if you suspect you may have gallstones, and further indicates the importance of consulting a doctor for official diagnosis. Fewer than half the number of people who actually have gallstones even experience symptoms.

Note if you experience biliary colic. Individuals with gallstones may experience a recurring pain in the upper right area of their abdomen (right upper quadrant pain) or in front of the lower part of their sternum (epigastric pain). There may be a gnawing pain, nausea and vomiting. The pain, known as biliary colic, usually lasts for more than 15 minutes and can sometimes radiate towards the back. Patients will usually experience recurring episodes of biliary colic after their first time experiencing the pain. In addition, biliary colic often occurs and then goes away. You may only feel this pain several times per year. This symptom can be easy to confuse with other digestive or abdominal pains. If you think you suffer from biliary colic, make an appointment to see your doctor.

Pay attention to how you feel after you eat a large or fatty meal. Observe whether you have abdominal pains and/or biliary colic after eating large or fatty meals, for example like a greasy breakfast with bacon and sausage or a big holiday meal like on Thanksgiving. These are the moments when you are most likely to experience pain and/or biliary colic. In some patients, minor biliary colic, without signs of infection, can be tolerated without medical intervention.

Watch for severe abdominal pain that spreads into the back or shoulders. This is the main symptom of gallbladder inflammation, which is often caused by gallstones. The pain usually worsens when drawing a breath. You may experience pain between your shoulder blades and in your right shoulder specifically.
Test for fever. Gallbladder inflammation is much more serious than biliary colic, and fever is the best way to distinguish between the two symptoms, based on their severity. You should seek medical attention right away if you fear that you have gallbladder inflammation. Infection develops in about 20 percent of patients, with a higher rate for diabetes patients. Infection can lead to gangrene and perforation of the gallbladder. Jaundice can also accompany fever. Jaundice can present with yellowing of the whites of the eyes (sclera) and skin.
Understanding the Risk Factors
Note the impact of age. The risk of developing gallstones increases with age. In fact, gallstone incidence peaks when a person is in his sixties and seventies.
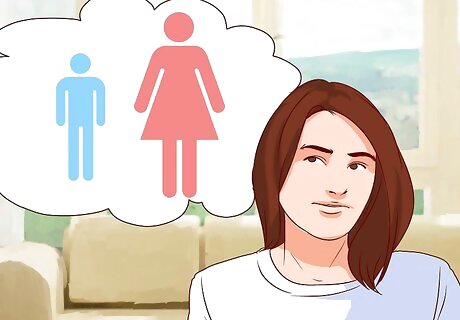
Understand the role of gender. Women are more likely to be diagnosed with gallstones than men; there is a 2-3: 1 ratio in this regard. Twenty-five percent of women will have a gallstone by the time they turn 60. This gender imbalance is due to the effect of the hormone estrogen, which women have more of. Estrogen stimulates the liver to remove cholesterol, and many gallstones are made from cholesterol. Women who take hormone replacement therapy pills experience an increase in risk of gallstones due to the estrogen. Hormone therapy can double or triple your risk of developing gallstones. Similarly, the birth control pill can also contribute to gallstone formation because of its effect on women's hormones.

Realize that pregnancy is a risk factor. Expect increased likelihood of gallstones if you are pregnant. Pregnant people are also more likely to develop symptoms, like those listed above, than their counterparts who are not pregnant. Seek a doctor’s opinion immediately if you suspect biliary colic or gallbladder inflammation. Gallstones may disappear after the pregnancy without surgery or medicine.
Pay attention to genetic markers. Northern Europeans and Hispanics are high-risk groups for gallstones. Some Native Americans, especially tribes in Peru and Chile, have very high instances of gallstones. Family history may also matter. Having a family member with gallstones may indicate you have a higher risk. However, studies are not yet conclusive regarding this risk factor.
Consider pre-existing medical conditions or diseases. Consult your doctor if you suffer from Crohn’s disease, cirrhosis or blood disorders as these are all risk factors for gallstones. Organ transplantation and prolonged IV feeding may also lead to gallstones. Individuals with diabetes are also at a high risk of developing both gallstones and gallbladder disease, without stones. This is likely due to weight and obesity.

Be aware that lifestyle factors are also risk factors. Obesity and frequent crash dieting have been found to increase the risk of gallstones by 12 to 30 percent. In obese people, the liver produces more cholesterol, and approximately 20 percent of gallstones are formed from cholesterol. In general, gaining and losing weight frequently can cause gallstones. The risk is highest for people who have lost more than 24 percent of their body weight and those who lose more than 3.3 pounds per week. In addition, diets that contain high levels of fat as well as cholesterol can be the basis for the formation of cholesterol gallstones (the most common type of gallstone that appears yellow). If you are inactive and lead a sedentary lifestyle, you are at higher risk for gallstones.

Note that certain medications can affect gallstone development. The use of birth control pills at an early age, high doses of estrogen replacement therapy, chronic use of corticosteroid or cytostatic therapies, and drugs used to lower cholesterol can increase the likelihood that you will develop gallstones.
Diagnosing Gallstones Medically

Undergo an abdominal ultrasound. Ultrasound is the best test to diagnose and differentiate gallstones. It is a painless imaging technique in which sonic waves produce an image of the soft tissues in your abdomen. A trained technician can find gallstones in the gallbladder or common bile duct. This test can detect gallstones in approximately 97% to 98% of individuals. The ultrasound procedure consists of a harmless machine that recreates an image of your gallbladder by reflecting inaudible sound waves against your body. Your ultrasound technician will apply a gel to your abdomen that will help the sound waves to travel through your body and be detected more accurately. This painless procedure is usually completed within 15-30 minutes. You should not eat for 6 or more hours before the test.

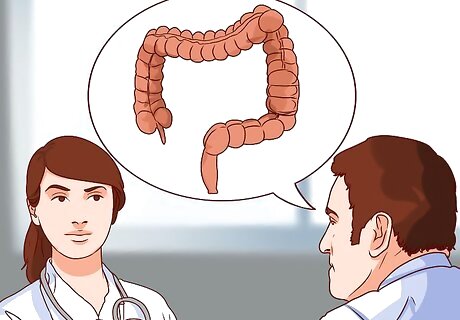
Schedule a computerized tomography (CT) scan. If your doctor wants still images of the area or the ultrasound did not produce a clear picture, a CT scan may be necessary. The CT scan will generate a cross-sectional image of your gallbladder by using special x-rays that will be interpreted by a computer. You will be asked to lie down in a cylindrical, donut-shaped machine that will scan your body for approximately 30 minutes. The procedure is relatively quick and will not be painful. In some cases, the doctor may prefer to use a magnetic resonance imaging (MRI) machine, rather than a CT scanner. This type of imaging involves a similar setup and will use changes in magnetic fluctuations to create an accurate image of your internal organs. This procedure may last up to an hour, and will involve you lying down inside a cylindrical scanning device. There is no advantage of a CT over an ultrasound, except that a CT may distinguish a stone in the common bile duct, the small tube that carries bile from the gallbladder to the intestine.
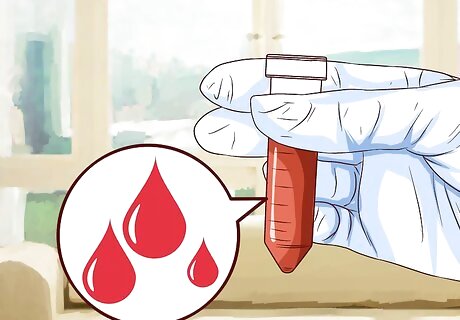
Get a blood test. If you suspect you may have an abdominal infection, you can get a blood test called a complete blood count (CBC). The blood test can establish whether a larger infection in the gallbladder may require surgery. Blood tests can also reveal other complications caused by gallstones in addition to infection, including jaundice and pancreatitis. This blood test is a standard blood test. Your healthcare provider or a technician will utilize a small needle to draw blood from your veins into small vials that will be analyzed by a lab for the doctor’s requested information. Leukocytosis and elevated C-reactive protein are indicators that are associated with acute cholecystitis, an inflammation of the gallbladder that could be caused by gallstones. Your doctor may check these levels as well as the standard panel of electrolytes and complete blood count analysis.
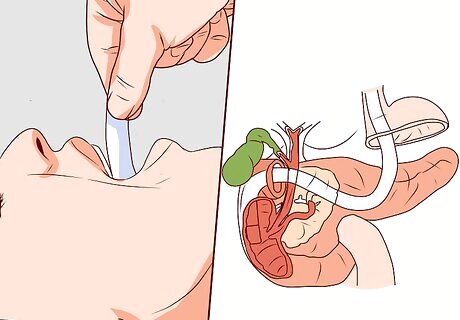
Undergo an endoscopic retrograde cholangiopancreatography (ERCP). Your doctor may recommend an ERCP, which is an invasive procedure in which a flexible tube about the thickness of a finger is placed into your mouth and down your digestive tract to examine parts of your stomach and intestine. If the physician finds gallstones during this somewhat invasive procedure, they can be removed. Let your doctor know all your medications, especially if you are taking insulin, aspirin, blood pressure pills, coumadin, heparin. These medications can affect bleeding during certain procedures, and you may be asked to adjust your medication routine. Due to the invasive nature of the procedure, you'll receive medication that may make you drowsy, and it is advised that you have someone who can accompany you or take you home after the procedure.
Rule out gallstones during liver function tests (LFT). If your doctor is already prescribing tests for possible liver disease or cirrhosis, he can check for gallbladder problems at the same time by determining if any imbalances are present. This test can be requested at the time of a blood test to provide further evidence of suspected gallstones. Your doctor will check your bilirubin levels, gamma-glutamyl transpeptidase (GGT) levels, and alkaline phosphatase levels. If these levels are elevated, you may have gallstones or another issue with your gallbladder.
Preventing Gallstones
Lose weight slowly. If you're trying to lose weight, don't do any crash dieting. Aim to eat healthy, well-balanced meals that include plenty of fresh fruits and vegetables, complex carbohydrates (like whole wheat bread, pasta, and rice), and protein. Your weight loss goal should be to lose one to two pounds per week and not any more than that. Losing weight slowly but steadily can lower the risk of gallstones.
Reduce your consumption of animal fats. Butter, meat and cheese may contribute to a diet that increases cholesterol and causes gallstones. Elevated fat and cholesterol contribute to cholesterol gallstones, yellow gallstones that are the most common type seen clinically. Instead, choose monosaturated fats. These fats increase your level of “good cholesterol,” which can reduce your risk of developing gallstones. Choose olive and canola oils over saturated animal fats like butter and lard. Omega-3 fatty acids, found in canola, flaxseed, and fish oil, may also help lower the risk of gallstones. Nuts are also healthy fats, and some research suggests that you may be able to reduce your risk of developing gallstones by eating peanuts and tree nuts, like walnuts and almonds.

Eat 20 to 35 g of fiber each day. Fiber intake can lower risk of gallstones. High fiber foods include legumes, nuts and seeds, fruits and vegetables, and whole grains. You should not have a difficult time getting enough fiber through diet alone. However, you can also consider taking fiber supplements, like flaxmeal. For a quick fix, combine one heaping teaspoon of flaxmeal in a glass of apple juice (eight ounces).

Choose your carbohydrates carefully. Sugar, pasta and bread may contribute to gallstones. Eat whole grains, fruits and vegetables to lower your risk of gallstones and gallbladder removal. Some research has suggested an association between high carbohydrate intake and increased incidence of gallstones. This is because carbohydrates are converted to sugar in the body.

Drink coffee and alcohol in moderation. Some research suggests that drinking coffee daily and drinking alcohol in moderation (one to two drinks a day) can result in a reduced risk for gallstones. The caffeine found in coffee stimulates gallbladder contractions and lowers cholesterol in bile. However, other caffeinated beverages, like tea and soda, do not appear to have the same effect, according to the research. Studies have found that drinking even one ounce of alcohol a day can reduce the risk of gallstones in some people by 20%.


















Comments
0 comment