views
- See a doctor for any kind of rectal bleeding. It’s not an emergency if it’s only a few drops of bright red blood when you wipe, though.
- Go to the doctor ASAP if you have black or dark red bowel movements and you have a fever, sharp pain, trouble breathing, dizziness, or weight loss.
- Treat minor rectal bleeding by consuming more fiber, drinking water, and taking it easy. Use hemorrhoid cream or OTC pain medication as needed.
Identifying the Type of Rectal Bleeding
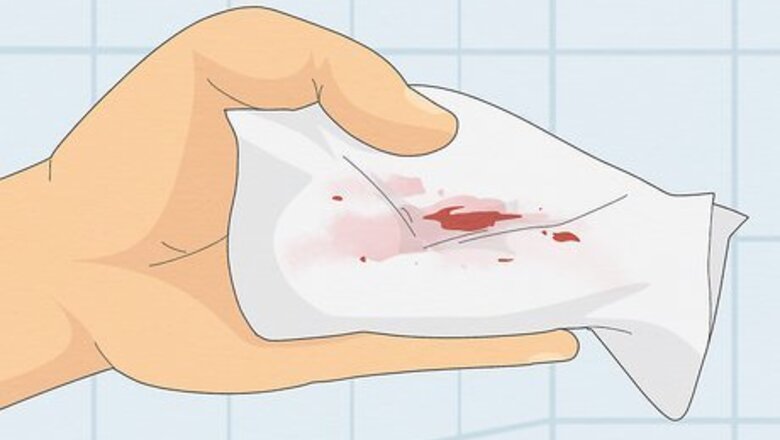
Check for bright red drops on toilet paper, which indicate minor issues. If you have minor rectal bleeding, you’ll see small drops or smears of blood on your toilet paper or in the toilet bowl. This indicates that you’re bleeding from your lower rectum, which actually isn’t the end of the world and will likely go away on its own. Still get it checked out soon, but you aren’t in danger. Minor rectal bleeding may indicate: Hemorrhoids. These are swollen veins inside or outside of the anus that can cause itching or pain while passing stool. These are extremely common. Anal fissure. This is a tear in the lower rectum. You’ll likely have a sharp pain while pooping, followed by a low burning sensation. An STI or irritation after anal sex. If you have genital warts in your anus, or you have anal sex without proper lubrication or preparation, it can cause temporary rectal bleeding. A side effect of blood thinners (like warfarin). This is especially likely if you have zero pain associated with the blood.

Look for bright, slimy blood mixed in stool (which is typically a minor problem). If you see streaks of bright red blood mixed into your stool when you wipe, attached to your stool in the toilet bowl, or coagulating together in the water, it indicates bleeding slightly higher up in your lower colon or rectum. These problems are usually minor, but can occasionally indicate something serious. You could have: An anal fistula. This is a small connection from an infected gland to your skin. You’ll often have yellow slime alongside blood and frequent anal pain. Gastroenteritis. If you feel sick or feverish, it’s probably just a tummy bug. IBD or Crohn’s disease. If you feel bloated and have bloody diarrhea, you likely have one of these chronic conditions. Bowel polyps. These are small growths in your intestine that occasionally bleed. This could be nothing, or an early warning sign of colon cancer.
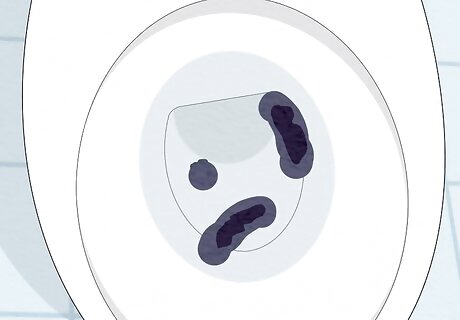
Search for dark red or black stool, as this is a sign of upper GI bleeding. Rectal bleeding isn’t always as apparent as blood-stained toilet paper. If the poop is black or the blood in your stool is a deep, dark maroon, then the bleeding in your upper digestive tract. This is much more serious and you should see a doctor ASAP. This could be: Internal trauma. You may have internal bleeding in your small intestine, stomach, or esophagus if you were in a car crash, fight, or fall. Colon cancer. Other signs include: trouble emptying your bowel, weakness, fatigue, radical changes in your bowel habits, and unexplained weight loss. Ulcer. You may have an ulcer in your stomach, intestine, or esophagus. If you have localized pain somewhere other than your rectum, this is likely the cause. Diverticular disease. These conditions are caused by bulges in your digestive tract. If you have a fever and nausea alongside the bloody stool, it’s probably a diverticular disease.

Reflect on your recent diet—red or black foods can change stool's color. If your poop just generally looks red or dark, you’re likely not bleeding—especially if you have no other symptoms and you’re not in pain. Eating a lot of black licorice, blueberries, beets, blood sausage, or foods with red food coloring can change the color of your bowel movements. This can also be caused by: Iron supplements or medication. Activated charcoal supplements. Pepto-Bismol.
Working with Your Doctor
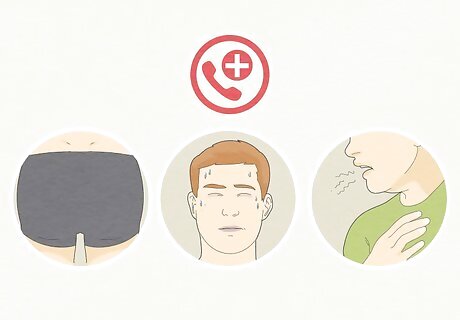
Schedule an appointment if you experience rectal bleeding. Any time you experience rectal bleeding, it is important to visit your doctor and have any serious causes ruled out or identified. Contact your primary care provider to make your appointment. Seek emergency medical care if you have black or dark maroon stools and you experience one of the following: You have rectal bleeding that is persistent associated with sharp pain that doesn’t dissipate. Your skin turns pale and sweaty while you are experiencing rectal bleeding. You have trouble breathing, blurred vision, you feel faint, or you’re nauseous. You’re confused, cold, or unable to urinate.
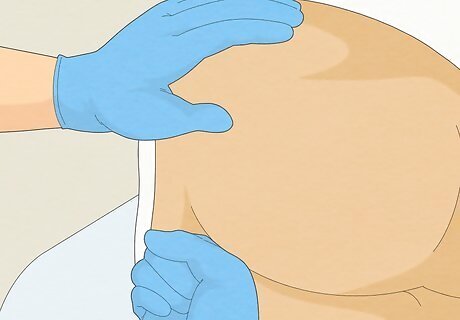
Ask your doctor about taking a rectal or stool exam. As an initial test, your doctor may perform a digital and/or visual examination. The doctor will use a gloved finger to inspect your anus and lower rectum for trauma, hemorrhoids, or the presence of a foreign body. The doctor may also feel and apply pressure to your abdomen externally. They’ll feel for any odd lumps or potential tumors inside your body. This may sound scary, but it won’t hurt. It may feel a little awkward to you, but remember that this your doctor’s day job. They’ve done this hundreds of times and you have nothing to be embarrassed about.

Agree to provide stool or blood samples for further testing. If the visual examination proves inconclusive, the doctor may request a sample of blood, stool, or both. A blood test will allow the doctor to determine how much blood you have lost and if your blood is able to clot adequately. The stool sample will be analyzed for bacteria and proteins to see what’s causing the bleeding. Both the blood sample and stool sample will need to be sent to an off-site lab for examination. The results may take up to a week to be returned.

Agree to receive a colonoscopy, if necessary. In some cases, your doctor may decide that a colonoscopy is needed to determine the cause or location of your rectal bleeding. When performing a colonoscopy, the doctor will insert a flexible plastic tube with a camera attached into your rectum. This allows the doctor to have a clearer image of your rectum and will allow them to determine the cause of your rectal bleeding. Instead of a colonoscopy, the doctor may ask you to complete an endoscopy instead, which will go through your mouth instead of your anus. If you’re 40 or older, your doctor will recommend regular colonoscopies to rule out the possibility of colon cancer.
Work with your doctor on a treatment plan once you have a diagnosis. If the source of your bleeding is minor, you’ll be able to treat it at home per your doctor’s instructions. However, if your bleeding is the cause of something more serious and/or the bleeding is higher up in your GI tract or stomach, work with your doctor to explore your options. You may need radiation or surgery to remove a tumor, remove your colon (called a colectomy), or stitch an internal wound shut. Your doctor may suggest a specific set of medications and antacids to neutralize an ulcer or soothe a GI bug. You may need to change your diet. The treatment for some diverticular diseases is a short-term liquid diet, for example. Celiac’s disease requires a gluten-free diet. Regardless of whatever your underlying condition is, your doctor will have a ton of resources to help you get back into tiptop shape.
Treating Minor Rectal Bleeding

Take any prescribed medications as directed by your doctor. Your doctor may give you a number of different medications, depending on the specific causes of your rectal bleeding. This might be a stool softener, pain medication, an iron supplement to increase your body’s blood production, or a medication to constrict blood vessels and decrease bleeding. If you have hemorrhoids, the doctor may also provide a hemorrhoid cream or a steroid cream to reduce rectal inflammation.
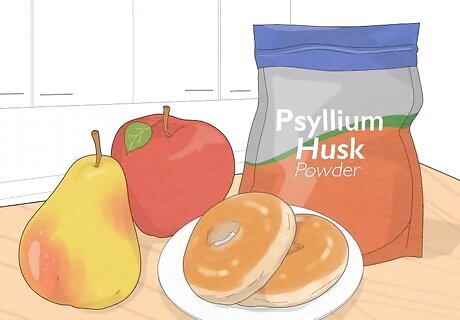
Include more fiber in your diet to sooth your bowels. A fiber-heavy diet is the absolute best solution for minor rectal bleeding. Anal fissure, hemorrhoids, tears, and general irritation will all be soothed by taking 25-30 grams of fiber a day. This will help your bowel movements pass more easily, which will give your rectum and GI tract time to heal naturally. Fibrous foods include: Legumes like lentils, split peas, and chickpeas. Fruits like pears and apples, with the skin on. Whole-grain muffins, bagels, and pasta. Oatmeal flakes. Granola. You can always take psyllium husk (like Metamucil) if you can’t eat enough fiber in your diet.
Drink enough water to keep your body hydrated. When your body becomes dehydrated, it will produce firmer stools that are harder to pass. Anal fissures and mild rectal bleeding are a common consequence of painful stools. Avoid this by staying hydrated so that your stools are easy to pass and do not damage your rectum or any hemorrhoids. On average, an adult woman should drink about 11.5 cups (2.7 L) of water and other fluids a day. An adult man should drink about 15.5 cups (3.7 L) of water and other fluids a day.

Wait for minor bleeding from fissures or hemorrhoids to stop on its own. Most instances of rectal bleeding from anal fissures will stop on their own once your bowel movement is over. If you have seen the doctor and know that your bleeding is the result of a minor issue, such as a fissure or hemorrhoid, wait for the bleeding to stop. In the meantime, avoid foods that you know cause you stomach pain, diarrhea, or constipation. Just eat a healthy, diverse diet with plenty of fiber.
Apply an over-the-counter cream for exterior irritation. If rectal bleeding from hemorrhoids or anal fissures persists over 2 or 3 days, visit your local drugstore pharmacy for a hydrocortisone or hemorrhoid cream (like Preparation H). The cream will decrease the discomfort or pain and help the sores or fissures heal. Consult your doctor before applying a medicated cream. Although most over-the-counter creams are mild and safe, your doctor will be able to advise you about which brand of cream to use. The doctor can also write you a prescription if a stronger cream is needed. There may be a slight increase in the burning sensation at the time of application, but it will be over in a few minutes.
Stop straining when you use the bathroom. If you push super hard when you have a bowel movement, stop doing it. Just give yourself longer to use the bathroom, or go back to use the toilet again in a few minutes or hours as needed. Straining and squeezing puts stress on your GI tract, which can make a minor issue worse.


















Comments
0 comment