
views
X
Expert Source
Marc Kayem, MDOtolaryngologist
Expert Interview
Symptoms of sleep apnea include snoring, waking up in the middle of the night, and fatigue after a full night’s sleep. You can do an at-home sleep apnea test from the comforts of your own bed to find out if you may be at risk. This is a great way to avoid spending the night at a sleep center. Before you can do this though, you’ll need to get an exam and talk to your doctor about your sleep habits and to find out more about your risk for sleep apnea.
Taking a Home Sleep Test
Get a referral to see a sleep doctor to get the testing equipment. Schedule an appointment with your doctor and tell them that you want to perform an unattended sleep study. They will refer you to a somnologist, which is a doctor that specializes in sleep issues. They will examine you and provide the home sleep study equipment (called an HST kit).Tip: The equipment you get from your doctor will come with instructions. If any of the directions differ from the steps here, follow your kit’s instructions instead. You can theoretically purchase the equipment yourself, but you won’t be able to interpret the results accurately. These machines usually cost $200-300, so it’s really not worth trying without a doctor. The sleep specialist may try to get you to have an attended sleep test, which is done at a hospital or sleep clinic. You can explain that a sleep center makes you anxious or you want to do it at home first before going to a clinic if they’re pushy about it.

Set the HST kit up at night right before you go to bed. Wait until you’re finally tired and ready for bed. Make sure that you set aside at least 8 hours of sleep to get accurate results from your test. Avoid drinking alcohol before bed. If you have any prescribed medications you take at night, talk to your doctor to see if you should take a night off or continue to take the medication.

Secure the monitor to your chest using the elastic straps. After your doctor gets you the HST device, you’ll have to take it home and secure it to yourself. The monitor comes equipped with elastic straps and bands. Slide the kit around your torso and secure these straps around your chest. Orient the machine so that it sits on top of your ribs. In most cases, the apnea monitor should fit snuggly above your stomach and at the lower part of your breast bone. Your doctor may give you a more complicated piece of equipment called a polysomnography machine. This kit has additional sensors to monitor your heartrate and brain activity. For these kits, you may need to attach a sensor to your heart or temple.
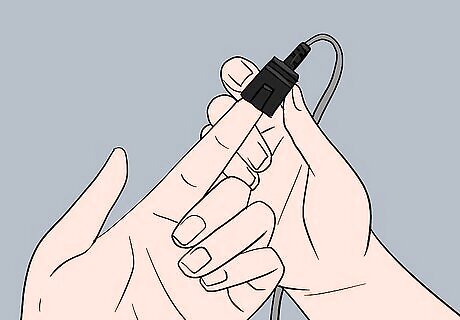
Put the finger monitor on by clipping it onto your index finger. The finger monitor is a small device with a plastic clip at the end. Open the clip and slide it over your index finger on either hand. The monitor keeps track of your heart rate during sleep. Without data from the finger monitor, you won’t have the information you need to determine if you have sleep apnea. Some HST kits have a small sensor that wraps around your finger instead.

Slide the breathing monitor on the elastic tube into your nostrils. There is a clear tube sticking out the top of the machine with a loop at the end. Slide the loop over your head so that the breathing tubes are in the front. Insert the two openings on the breathing tubes into your nostrils. Take time to make sure nasal tubes are completely secured. This is the piece of equipment that is most likely to fall off while you sleep. You can usually tighten a strap on the tube to secure it to the back of your head.

Turn on the monitor after you lie down in bed. When you’re ready to go to sleep, press the “on” button on your monitor. Depending on the model of the device, the button will look different or be positioned in a different location. However, your doctor should instruct you on which button to press. Most HST kits will chirp or beep when the test is starting. Once the test begins, do not turn the unit off to ensure that you get a complete data set.

Fix the tubes or straps if you wake up and they've fallen off. Before you go to sleep, check to see that the monitor, nasal tubes, and finger clip are still attached properly. This is important, as some parts of the monitor could come loose from your body while you sleep. If you do wake up in the middle of the night, check the components again. Put the tubes or clip back where they belong if they fall off in the night. You may need to do this for 2-3 nights depending on your doctor’s instructions.
Returning the Monitor and Getting Your Results

Remove your monitor when you wake up in the morning. Once you wake up in the morning, switch the monitor off by pressing the same button you used to turn it on, and carefully remove each piece of equipment from your body. Put the monitor, tubes, and sensors to the container they came in.Tip: If you have to take the test for more one night, give the tubes and breathing monitor a thorough cleaning with a disinfectant wipe. Then, put the kit away after each night to make sure you don’t lose any tubes or straps.
Return the monitor to the sleep doctor or diagnostic company. After you've concluded your sleep test, you need to return the monitor to the sleep doctor or diagnostic company in a timely manner. This might include dropping it off at their office or mailing it in. It is important to return the monitor as soon as possible, so you can get results back quickly. Your doctor may instruct you to return the monitor the morning after your test. These kits are pretty expensive, so be careful when you take it back to your doctor!
Wait a few days or weeks for your results to come back. Depending on your method of returning the monitor, it could take from several days to several weeks to get your results back. During this time, a diagnostic service company will download the data from the HST monitor, analyze the results, and send a report to your doctor, who will make a formal diagnosis.

Meet with your doctor to go over the results. You’ll get a few different results back from your at-home test. Some of these results will be fairly straightforward, like your pulse, temperature, and oxygen levels. The key result is your AHI, which stands for apnea/hypopnea index. This is a cumulative score that assesses the severity of your breathing issues while asleep. Generally speaking, you do not have sleep apnea if you score under 5 AHI. A score of 5-15 indicates a mild case of sleep apnea. Anything higher than 30 is considered severe and requires immediate treatment. Your somnologist will be able to go over your treatment options if your AHI is higher than 5.
Evaluating Your Sleep Apnea Risk

Complete a sleep apnea questionnaire online to assess your risk. There are 2 scientifically valid tests that you can take at home on your computer to see if you’re at risk for sleep apnea: the Epworth Sleepiness Scale test, and the Berlin Sleep Questionnaire. These tests gauge the severity of your snoring, fatigue, and sleep habits. Take both of these short exams to determine if you’re at risk of having sleep apnea or not. You can take both of these exams on the American Sleep Apnea Association’s website. Scoring high on either of these exams does not automatically mean that you have sleep apnea. Don’t worry if your scores are high—these tests are just an initial assessment.

Use a BMI calculator to determine if your weight is a risk factor. Sleep apnea is fairly uncommon in people that are not overweight or obese. To determine if your weight is putting you at risk, use a BMI calculator to find your Body Mass Index, which is the scale used to determine healthy weight levels relative to your size. If your BMI is 35 or higher, you are at high risk for sleep apnea.Tip: If you are overweight, you can reverse your chances of getting sleep apnea by dieting, exercising, and taking care of your body. Shedding a few pounds is one of the best ways to avoid sleep apnea. You can find your BMI using the National Heart, Lung, and Blood Institute’s calculator here: https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm.

Stop smoking and limit sleeping pills and alcohol to avoid sleep apnea. You are much more likely to develop sleep apnea if you smoke cigarettes, drink alcohol before bed, or take sleeping pills regularly (even OTC medications, like Benadryl). If any of these apply to you, you’re putting yourself at risk of sleep apnea. Talk to your doctor about your alcohol consumption and see if you can get help to quit smoking. Try developing better sleep habits by going to bed earlier and limiting screen time before bed. Men are also roughly twice as likely to suffer from sleep apnea. You’re also more likely to develop sleep apnea the older you get.
When to Seek Medical Care

Consult your doctor if you suspect you have sleep apnea. Talk to your doctor after taking a sleep apnea questionnaire or if your snoring is very loud. Additionally, work with your doctor after you do an at-home test. They’ll help you get properly tested so you can get the right treatment. If you took a questionnaire, bring your results with you when you see the doctor. They’ll go over your questionnaire with you.

See a specialist if your doctor recommends it. After you get the results of your sleep apnea test, your doctor may refer you to a specialist. Follow your doctor’s advice to make sure you get the right treatment. You may need to see multiple specialists to get a complete diagnosis. You may need to see a sleep specialist to confirm your doctor’s initial diagnosis. Depending on the suspected cause of your sleep apnea, your doctor might refer you to an ear, nose, and throat (ENT) specialist.

Use the treatments provided by your doctor if you have sleep apnea. If you have sleep apnea, don’t worry. There are plenty of options available when it comes to treatment and the condition is extremely manageable. Talk to your doctor about your treatment options to find the solution that’s right for you. Possible treatment options include: A continuous positive airway pressure (CPAP) machine that blows air into your nostrils while you sleep to make sure your breathing is uninterrupted. A bilevel positive airway pressure (BPAP) machine, which is similar to a CPAP machine but provides less pressure while you exhale. An oral device can bring your jaw forward to open up your airways. Surgery to open your airways up, but only in extreme cases.



















Comments
0 comment