
views
Chennai: Not only do medical students in India lack a crucial ability to relate emotionally with their patients, but those from private high schools are worse at it than those from government high schools, a recent survey, conducted on students in a medical college in Chennai, revealed.
There’s something rotten in the state of medical education and care in the country, stemming from a deep deficiency of emotional intelligence (EI) among medical students, the survey, conducted by researchers Subhashini Sundararajan and Dr. Vijayaprasad Gopichandran from Chennai’s ESIC Medical College & PGIMSR, found.
Published in the journal BMC Medical Education, the survey of 207 medical students found that those who came from government schools consistently had greater emotional intelligence than those from private schools, something Gopichandran had observed as a teacher at ESIC.
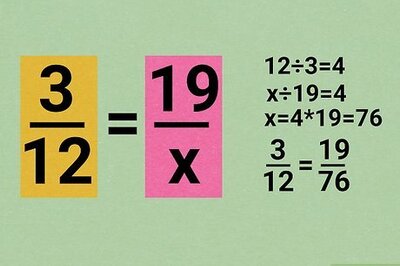
Students on an average scored 107.58 out of a maximum score of 160 for EI, with government school students consistently scoring more. The study found that factors like age, gender, urban/rural nativity did not have as significant an impact on the scores, as much as schooling did.
The survey held the “collectivist social setting” of government schools and the stress on individualism in private schools responsible for this.
“Government schools across the country suffer from resource deprivation and students have really struggled. Their learning ends up happening in a collective, collaborative kind of manner, “ Gopichandran elaborated on how such a survey could have similar results all over
India.
“Kids from the best private schools have trouble adapting to a medical college, and in coping with how difficult their course is, because they’re not comfortable studying collectively,” he added. Students from government schools band together more easily, sharing notes and the burden of work, and offering help, while private school kids are mostly seen trying to study on their own with earphones on.
This, he pointed out, has become more noticeable post the NEET exam, with dramatically reduced the number of students from government schools entering medical colleges.
Such behaviour may be indicative of how students interact with patients once they start practicing medicine. The inability to listen to a patient has damaged the trust implicit between the doctor and the patient. Previous studies, said Gopichandran, showed that
if a patient is allowed to talk uninterrupted for two minutes, it dramatically reduces the overall time needed to give a correct diagnosis.
“Emotional intelligence does not take time,” he said refuting arguments that doctors in India’s government hospitals don’t have the time to emotionally invest in patients. “It is a matter of a couple of minutes, of the correct body language, the ability to listen, a simple hand on the patient’s shoulder,” he said, drawing from his own practice and from that of his mentors during his student days.
Unfortunately, students now don’t get to interact with such doctors. They’re few and far in between and students mostly learn from the colder behaviour of their own teachers.
“The rise of specialty and super specialty practices has meant that there are very fewer general physicians practicing ethical medicine. Patients aren’t seen as whole people but as organs,” said Gopichandran. “I can’t blame the students,” he added, “they’re responding
to a market that only rewards those with most degrees.”
As his survey pointed out, private school students were deeply uncomfortable with getting to know their patients fearing their objectivity would be lost. They also thought of anger and a paternalistic attitude towards patients as necessary tools to make them stick to treatment regimes.
In such cases, the doctor and the patient tend to get trapped in a vicious cycle of diminishing trust, each responding negatively to the other. As the survey pointed out, this has led to a rush of violent attacks on doctors by patients and their attendants in the past few years.
However, “emotional intelligence is a cognitive process,” Gopichandran told News18, adding that it can be taught, something he himself learnt from researchers at the Tata Institute of Social Sciences who are teaching EI to policemen.
On the basis of this survey, Gopichandran and Sundarajan, who is his student as well has the lead author, are preparing a policy brief for the National Medical Council (NMC), to incorporate EI into medical training. Not as a separate lecture, he said, but as part of every course and for every teacher to impart.
“There has to be a focus on primary healthcare and on pushing students to explore medicine instead of fast-tracking their careers to corporate hospital jobs.” Gopichandran said. Lamenting that there is no joy left in medicine anymore, the researcher stressed that such attitudes needed changing.
















Comments
0 comment