
views
X
Trustworthy Source
National Health Service (UK)
Public healthcare system of the UK
Go to source
However, trichomoniasis can only be diagnosed by a health care provider by running tests and can't be diagnosed by symptoms alone.
Recognizing Symptoms of Trichomoniasis

Monitor your vaginal discharge. For most women, vaginal discharge is perfectly normal and can range from being clear to milky white. Abnormal discharge will look greenish-yellow and frothy. A strong odour is also a sign of abnormal discharge. Trichomoniasis is spread through contact with vaginal discharge which happens most often during vaginal intercourse. However, non-sexual transmission can sometimes occur from penetration from other items like douche nozzles. Fortunately, the parasite can only last up to 24 hours outside of the body.
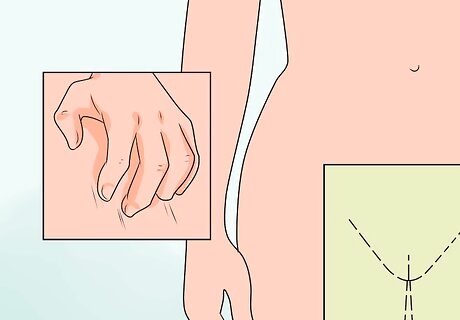
Recognize abnormal genital symptoms. Trichomoniasis can cause redness, burning, and itching sensations at the genitals in some infected individuals. These symptoms may indicate a possible trichomoniasis infection or that of another STI. Trichomoniasis causes irritation within the vaginal canal or vulva. Vaginal irritation can be normal if the irritation only lasts for a few days or gets better after treatment. However, if irritation persists or gets worse, it's best to talk to your doctor about it and get it properly diagnosed and treated.

Do not ignore painful or unpleasant sexual intercourse or urination. Trichomoniasis can cause inflammation and soreness in the genitals that can make intercourse uncomfortable. See a physician if you experience these symptoms, and do not participate in intercourse until you have been tested for STIs or STDs. Avoid all forms of sexual intercourse including anal and oral sex until you've been tested and cleared. You should also inform your sexual partner or partners if you suspect you have an STI/STD and encourage them to also get tested and treated. Some clinics will help you inform your partners anonymously by giving them a contact slip that lets them know they have been exposed to a sexually transmitted infection. It won't have your name on it and it won't necessarily tell them what the infection is.
Getting Tested and Treated for Trichomoniasis

Recognize when you are at risk of getting STI/STDs. With any sexual activity, there is always a risk of being infected by an STI. In some circumstances, you are more likely to receive an STI and knowing about these situations can help you and your health care professional decide if you need to get tested. You will probably need to be tested if: You have had unprotected sex with a new partner. You or your partner has had unprotected sex with others. Your partner tells you they have a sexually transmitted disease. You are pregnant or planning to be pregnant. Your doctor or nurse notices abnormal vaginal discharge or your cervix is red and inflamed.
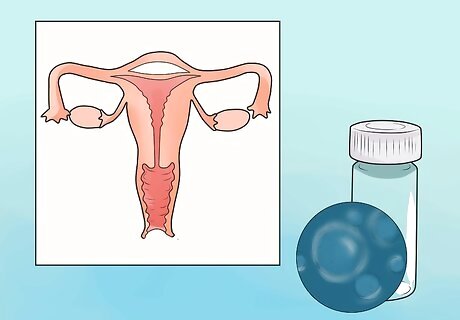
Allow your doctor to collect cell samples from your vagina to test for trichomoniasis. Your doctor or health care provider will ask to collect vaginal cell tissue or discharge from your vagina by using a cotton swab. Sometimes the swab may look like a plastic loop rather than a cotton tip. The tool is wiped over parts of the body that could be infected such as inside your vagina or around it. This is often painless with only a bit of discomfort. Your doctor might be able to immediately examine the sample under a microscope and let you know your results right away. Or you may have to wait 7-10 days for your results. During this waiting period, be sure to avoid any sexual activity so you don't spread an infection if you have one. Blood tests and cervical screening tests don't test for trichomoniasis. Be sure to ask specifically for a trichomoniasis or STI test.

Take antibiotics prescribed to you by your doctor if you do have trichomoniasis. If your test comes back positive, your doctor will prescribe antibiotics to treat trichomoniasis. At times, your doctor might even prescribe medication to you before your tests come in just in case. Your doctor will most likely prescribe you an oral antibiotic called metronidazole (Flagyl) which stops the growth of bacteria and protozoa (trichomoniasis is a protozoan parasite). Side effects include dizziness, headache, diarrhea, nausea, stomach pain, loss of appetite, constipation, changes in taste, and dry mouth. It can also cause your urine to come out darker in colour. Be sure to notify your doctor if you are or may be pregnant. Metronidazole is safe for pregnant women. Do not drink alcohol while taking these antibiotics. Contact your doctor if your side effects persist or worsen to a point where it disrupts your day to day life. Tell your doctor immediately or go to an emergency clinic if you experience seizures, numbness or tingling in your hands and feet, or mood or mental changes. Many women who have trichomoniasis also have bacterial vaginosis. Fortunately, the antibiotics used to treat trichomoniasis also treat bacterial vaginosis.
Preventing Trichomoniasis

Schedule routine checkups to ensure your sexual health. It is always important to get routine check-ups from your doctor or health care professional, even if you don't think you have any STIs. Remember, only 15-30% of trichomoniasis infected individuals show signs of infection. The other 70-85% never display any symptoms. If left untreated, trichomoniasis can increase your chances of getting HIV or increase the likelihood of transmitting HIV to your sexual partners. Trichomoniasis in pregnant women can cause premature ruptures of membranes that protect the baby and cause early delivery.
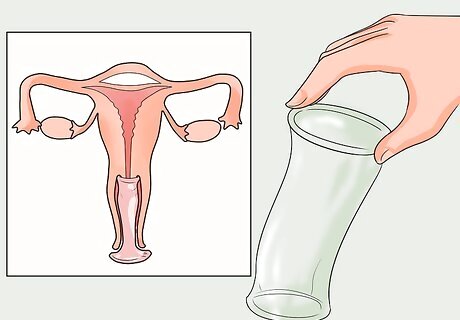
Practice safe sex. If you are not involved in a mutually monogamous relationship with an individual free of STDs, always use a latex condom (male and female) to help avoid contracting sexually transmitted conditions. Some more methods of protection include: Using condoms when engaging in oral, anal, and vaginal sex. Avoiding sharing sex toys. If you do share them, wash them or cover then with a new condom anytime anyone new uses it.

Alert any sexual partners to your infection. Notify sexual partners with whom you have had unprotected intercourse or direct genital contact so that they can be tested and treated if necessary. Some clinics will help you inform your partners anonymously by giving them a contact slip that lets them know they have been exposed to a sexually transmitted infection. It won't have your name on it and it won't necessarily tell them what the infection is but will urge them to get tested.
















Comments
0 comment