
views
X
Research source
Needless to say, having a vaginal prolapse can be a significant concern, both cosmetically and functionally. If your vaginal prolapse is mild, you may be able to treat it with a combination of activity modification, a vaginal pessary, Kegel exercises, and/or estrogen replacement therapy. If it is moderate to severe, however, surgery will most likely be required; the good news is that surgery is usually very successful at treating and resolving vaginal prolapse.
Treating Vaginal Prolapse Without Surgery

Change your activities to prevent stress to the vaginal walls. If you have only mild vaginal prolapse, your doctor will likely recommend modifying your activities to avoid heavy lifting and/or straining. This will reduce the stress on your pelvic floor muscles, and may help to improve (or at least to prevent worsening of) your vaginal prolapse. Keep in mind that surgery is not necessary with vaginal prolapse. You can leave the prolapse untreated without any negative impact on your health.

Consider trying a device meant to support the vaginal walls. Something called a "vaginal pessary" is a circular device, usually made of soft plastic or rubber, that is inserted into your vagina. The pessary will hold your vaginal structures in place, thus preventing symptoms of prolapse and/or worsening of your prolapse. You will need to see your doctor to discuss this treatment option and to have it inserted into your vagina. A vaginal pessary must be removed and cleaned at regular intervals. Your physician can instruct you on how to do this, as well as the frequency at which it needs to be done. Some women find vaginal pessaries uncomfortable, or find that they fall out and have difficulty keeping them in place. Try a pessary and to see how you feel with it in. You can evaluate from there whether you find it a helpful mode of treatment. Vaginal pessaries are more successful in women who are not sexually active than in women who are. If you are sexually active, you or your partner can remove the pessary for intercourse.
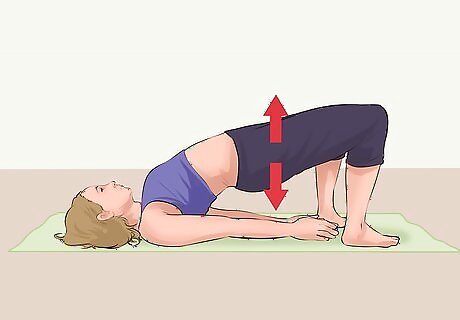
Perform Kegel exercises to strengthen your pelvic floor muscles. Kegel exercises strengthen the pelvic floor muscles - these function to support the uterus and vagina, as well as the bladder, the small intestine, and the rectum. Do Kegel exercises at least 3 times per day, ultimately aiming for 10 repetitions each time. Here's how to effectively perform Kegel exercises: To identify your pelvic muscles (the ones you will be flexing during Kegel exercises), stop urinating mid-stream. Notice which muscles you used to do this task - this feeling of muscle tightening is what you will be aiming for when you perform the exercises (which is recommended to do when you are not urinating - the urination test is simply used to allow you to identify the muscles). When lying down or sitting comfortably, contract your pelvic muscles and hold the contraction for 5 seconds. Then, release for 5 seconds, and then repeat this 5 times. Ultimately, you will want to aim to hold the contraction for 10 seconds, to release for 10 seconds, and to repeat this 10 times. Stay relaxed as you perform the exercise and do not hold your breath. Rather, continue to breathe deeply as you perform the exercises. Kegel exercises are not meant to be tiring; they are more about focus, as you keep your mind focused on the contractions that will effectively strengthen these muscles. If you have difficulty performing Kegels, then let your doctor know. You may need a referral to see a physical therapist for help. Kegels are also useful for preventing uterine prolapse.

Ask your doctor about estrogen replacement therapy as a method to treat vaginal prolapse. Many cases of vaginal prolapse occur following menopause. They are linked to the decreased estrogen that is present post-menopause, as a decreased estrogen level correlates to a weakening of the vaginal area and the surrounding muscles and ligaments. The most common way to deliver the estrogen is to insert an estrogen cream into your vagina, but any form of estrogen will work. However, keep in mind that homeopathic remedies cannot replace this therapy. Estrogen replacement therapy can help to prevent this natural weakening of the pelvic muscles and ligaments, and hence to reduce the risk of any further vaginal prolapse. Note that there are some cases in which estrogen replacement therapy is not safe. These include people with certain types of cancers whose growth may be fuelled by the presence of estrogen (such as many breast cancers), as well as those who are at an increased risk of blood clots and stroke, among other things. Your doctor will be able to go over the risks and benefits of estrogen replacement therapy in your specific case, to help you decide whether this treatment is right for you.
Opting For Surgery

Know that vaginal surgery is the mainstay of treatment for more severe vaginal prolapse. While strategies such as activity modification, pessaries, Kegel exercises, and estrogen replacement therapy can be helpful, moderate to severe cases of vaginal prolapse may need to be treated with surgery. The type and extent of the surgery will vary depending upon the type and severity of your prolapse. This is something that your surgeon will assess and discuss with you after he or she has performed a physical exam to thoroughly assess the extent of your vaginal prolapse. As you await surgery, you may be offered treatments such as a vaginal pessary to help control your prolapse until it can be corrected surgically. Also, keep in mind that there is no medical reason why surgery has to be done.

Ask about anesthesia during surgical procedures. Most people are put under general anesthesia while they undergo surgery for vaginal prolapse. Tell your doctor if you have had problems with general anesthesia in the past, or if you have a family history of problems tolerating anesthetic. Most people are completely fine with it; however, it is important to talk with your doctor about any concerns you may have. Some women just receive a spinal or an epidural for pain control during surgery. While general anesthesia is normally recommended, these are other options that can be considered.

Educate yourself about what to expect during surgery for vaginal prolapse. Vaginal surgery is the mainstay of treatment followed by laparoscopic surgery. In vaginal surgery, the surgery is conducted through the vaginal opening. In laparoscopic surgery, small instruments are inserted into the abdominal cavity though tiny incision points, with the help of a small camera that allows the surgeon to see during the operation. Unless there are complications, you will most likely need to stay in the hospital for one to two days following surgery. This will help to ensure that the initial stages of your recovery are going well. Recurrence after having prolapse surgery can be as high as 20 to 60%. To reduce your risk, be diligent about doing Kegels, limiting lifting, and any other preventative measure that your doctor suggests after surgery.
Recovering After Surgery

Avoid heavy lifting and other similar activities while you recover. In the first six to nine weeks after surgery, it is important to avoid heavy lifting, as well as any other activities that may increase the pressure or stress on your abdominal or pelvic areas. Ask your boss for modified duties at the workplace if you have a job that involves heavy physical labor. Your doctor may advise that you do Kegel exercises to strengthen the muscles in your pelvic area following surgery. Be sure to follow your doctor's advice on when to begin strengthening exercises, and how many to do at a time, so that you do not put undue stress on your pelvic area following surgery. Also avoid sexual intercourse for 6 weeks following surgery, to allow time for a full recovery.

Consider weight loss to prevent recurrence of your prolapse. If you are overweight or obese, this puts additional stress on the muscles and ligaments within your pelvis and vagina. Being overweight can significantly increase your risk of recurrence of the condition following surgery, due to the continual extra pressure in the area. Therefore, to minimize your risk as much as possible, and to ensure that the benefits of surgery last for as long as possible, you may want to consider weight loss. Strategies to reduce your weight (if you are overweight) include increasing your aerobic (fat-burning) exercise, and improving the health of your diet, among others. Click here for more information on how to lose weight safely and effectively if this is of interest to you. You will also want to ask your doctor to treat chronic conditions such as a persistent cough or ongoing constipation, which may put additional stress on your abdominal and pelvic floor muscles.

Be aware of your expected recovery from vaginal prolapse. While the specifics of recovery may vary on a case-by-case basis (depending upon the severity of your prolapse), surgery is generally very successful at treating vaginal prolapse. You can return to normal activity fully by six to nine weeks after surgery, and your surgeon can advise you on a plan for a gradual return to activity during this time period. Note that sexual problems may persist even after the surgery is complete. The surgery will most likely resolve the anatomic problem (the prolapse), but it will not necessarily resolve associated sexual challenges. If you are struggling to get your sex life back on track, you can ask your doctor for suggestions or for a referral to a physician who specializes in women's sexual health and wellbeing. Challenges that are common include pain with intercourse and decreased libido, among other things.

















Comments
0 comment