
views
Confirming Trigger Finger and Treatment

Visit your doctor. If you hear or feel a crackling or popping sound/sensation when you extend your finger or thumb, it is a good bet that you have trigger finger. However, it is vital that you have this diagnosis medically confirmed, especially if you have not had the condition previously. You need to rule out other, possibly serious, conditions. Your fingers extend and bend by way of tendons, which are essentially flexible bands that stretch and retract to move the attached bones. They are protected and lubricated by tendons sheaths (basically tubes). If a tendon sheath becomes inflamed (due to repeated use or another medical condition), it can narrow and cause the tendon to scrape or even get caught in place, causing the locking, popping, and crackling sensations of trigger finger. Being female and/or over age 40, and having diabetes or rheumatoid arthritis can make you more susceptible to trigger finger. Most often, though, it is suffered by people who use repeated gripping motions with their hand(s), such as carpenters, farmers, factory workers, and musicians. It is important to go to the doctor to diagnose trigger finger, because sometimes people mistake a fracture or dislocation for the condition. Your physician can determine the severity and proper treatment of your condition, and can also rule out potentially-dangerous infections that can occur at the site of inflammation.
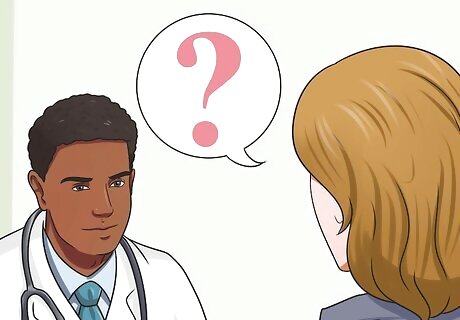
Discuss treatment options. Treatment for trigger finger can range from rest to surgery, depending on severity. Splinting is a common first-level treatment, especially for milder forms of the condition. Studies indicate that splinting for a period of around six weeks is roughly as effective as a cortisone shot in the joint, another common treatment for trigger finger. There are several types of splints and you can splint your finger continuously or only during times of rest. Talk to your doctor about the best treatment option for you.

Confirm that you can and should apply splints yourself. Before trying to splint your finger, confirm with your doctor that you can and should splint your affected finger(s) yourself. Self-treatment without proper medical advice is not recommended. Splint your finger temporarily until you can receive proper medical attention. Do not engage in long-term splinting on your own initiative, however. Improper or prolonged splinting can cause joint damage, obstructed blood flow, and/or skin infections.
Applying Buddy Splints

Know when to use the buddy splint. This splinting technique is often used for trigger finger when a finger ligament is strained or when a joint is dislocated. Buddy splinting is not suitable for unstable joints and/or fractured fingers. A buddy splint adjoins two fingers by taping them together, just like buddies. The fingers are taped at a point which is above and a point that is below the affected joint. Please note: contact your physician before engaging in long-term splinting for apparent trigger finger or any other condition.
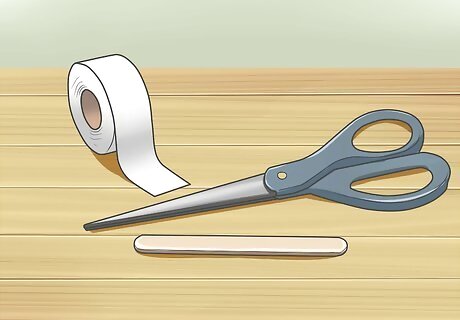
Prepare the necessary materials. Before you apply a buddy splint, you will need to gather some materials. You will need: Scissors. You will need scissors for cutting the medical tape and for cutting the wood pieces, if necessary. Two tongue depressors or Popsicle sticks. Any wood that is thick enough to support a finger will do. Typically, tongue depressors can be found in any local pharmacy — just make sure that it will support the entire length of the finger. Medical tape. This secures the wooden splint to the fingers. Micropore tape is easy and gentle for sensitive skin. If you want very adhesive tape, you can purchase Medipore or Durapore instead. If you do not have the tape at home, you can use thin strips of cloth about 4 to 5 inches long to secure the splint; however, medical tape is preferable. You will need a half-inch width cloth tape, which can be found at pharmacies near you.
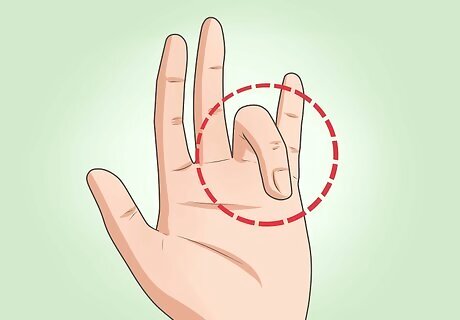
Determine what two fingers to buddy splint together. If the index finger is not broken or injured, avoid using it. It's your most useful finger and you don't want it hindered by the splint if it doesn't have to be. If the middle finger is affected by trigger finger, then choose the ring finger as the buddy. You want your hand as mobile as possible. If you can buddy with the ring or pinky finger, do so. You'll experience less inconvenience if your index and/or middle finger are free.

Place the splint under the trigger finger. Be sure to cover the entire length of the affected finger. After placing one tongue depressor (or similar device) underneath the finger, you should place another on top of the finger. Basically, your finger will be in the middle of a wooden stick sandwich. Trim the wood to size so that it does not catch/destabilize the splint once it is in place. You can buddy splint with just tape, but using a structural support like the wooden sticks makes the splint much sturdier and more effective. Only splint the injured finger — the buddy finger can be left alone.
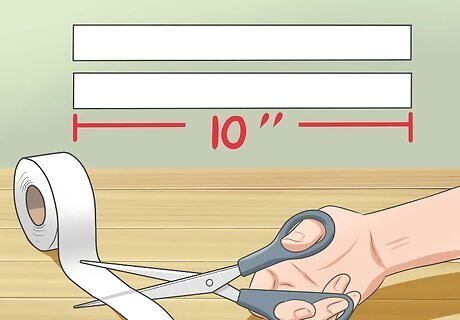
Grab your tape. Using the scissors, cut two pieces of tape, each measuring 10 inches (25 cm). Here's how to wrap your finger: Wrap the first piece of tape once around the trigger finger, in between the first and second knuckles. Bring the piece of tape around the buddy finger and wrap it firmly until the tape runs out. Repeat in between the second and third knuckle of the affected finger, and then around both fingers. If the your little finger (pinky) is affected, you must wrap it at the end of the finger, which will line up between the second and third knuckles of the ring finger.

Check the circulation of the buddy and affected finger. Pinch the nail of each finger for about two seconds. Does it return to a pinkish appearance within a couple of seconds? If so, good. The blood circulation is just how you want it. Your splint is then finished. If it takes more than two seconds, then your fingers are not getting enough blood because your splint tape is too tight. Removing and reapplying the buddy splint is the best thing to do in this situation.
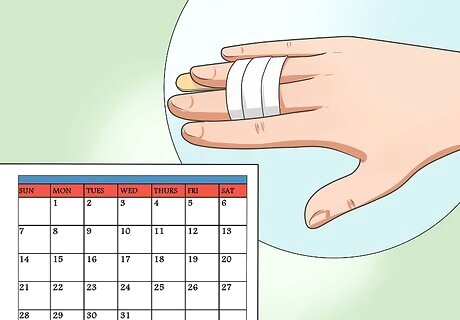
Wear the splint for four to six weeks, or as recommended by your doctor. In certain cases of trigger finger, it may take only two to three weeks to heal. However, the average time is a bit more. Ultimately, it depends on the extent and severity of the inflammation in the tendons of your affected finger. If you are lucky, your doctor will only recommend that you wear the splint at night or while otherwise resting. This is much less inconvenient than continuous splinting. Whether splinted at all times or just sometimes, avoid using your injured hand (and especially the injured finger) as much as possible. Immobilization is key to a speedy recovery. When the splint (and tape) is dirty or becoming loose, replace the splint with a new one. If after this period of time your trigger finger does not seem any better, consult your doctor again. He or she will conduct further assessment and properly treat your finger.
Utilizing Static Splints

Know when to use a static splint. Static splints support, protect, and straighten injured fingers by way of form-fitting piece of metal, plastic, etc. They are used in cases of trigger finger in order to hold a joint in place, regardless of whether it is just slightly bent or completely out of alignment. Since a proper fit is key to a static splint, it is best to accurately measure the length and diameter of the affected finger before choosing the splint. Static splints can be bought over the counter at pharmacies and supermarkets. They are made from basic metal, plastic and foam. Please note (again): You should consult your doctor first before using a static splint for anything less than short-term protection. Among other benefits, the doctor can help ensure that the splint is the proper type, size, and fit for your injury.

Put the splint on the trigger finger. Straighten the injured finger by supporting it with the other hand. Slowly slide the static splint along the underside of the trigger finger until it fits into place. Make sure to check if the static splint fits completely and the finger is really straight. If the finger is slightly bent either forward or backwards, it can lead to the development of sores at the knuckle.
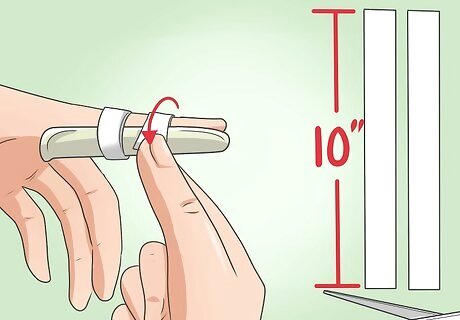
Cut your tape into two 10" (25 cm) pieces. Wrap the first piece of tape firmly once around in between the first and second knuckles of the trigger finger until the tape runs out. Repeat in between the second and third knuckle of the affected finger until the tape runs out.

Check the circulation of the affected finger. Do this by pinching the nail for about two seconds. If the nail returns to pinkish appearance within one to two seconds, then it has good blood circulation. If it takes more than two seconds, the blood flow is insufficient because the splint is too tight. Removing and reapplying the splint is the best option.

Use the splint for four to six weeks. This is the average time it takes a trigger finger to heal. For some people it will heal in only two to three weeks time; it depends on the extent and severity of the inflammation in the tendons. Make sure to change the tape twice daily or as necessary. Depending upon your injury and your doctor's advice, you may only need to use the splint while sleeping/resting. This is more convenient, of course, but full-time splinting will likely provide better protection and healing. When the splint and tape becomes soiled and dirty, replace it with a new one. If trigger finger does not resolve after four to six weeks, you should contact your primary health provider for further assessment and management
Employing Stack Splints

Know when to use a stack splint. These specialized preformed splints are used in trigger finger cases when the joint that is closest to the tip of the finger (called the distal interphalangeal joint [DIP]) is damaged or cannot straighten by itself. Stack splints (one common brand is known as Stax splints) come in various sizes. They are designed to fit over the DIP joint in order to prevent it from bending, while still allowing bending of the joint at the midpoint of the finger (the proximal interphalangeal joint [PIP]). Stack splints are usually made from plastic with holes for ventilation. They can be found in pharmacies or grocery stores and you can try to fit them there before purchase. Please note (once more): Despite their availability and relative convenience, it is always best to consult your physician before using stack splints to address trigger finger or another condition (such as mallet finger).
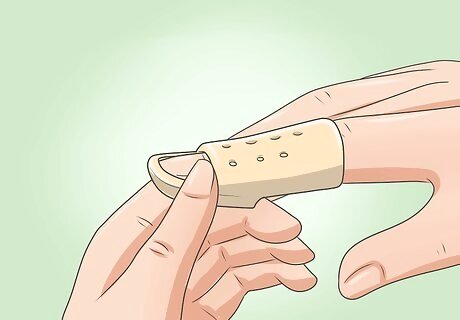
Place the splint on your finger. To do so, straighten the affected finger while supporting it with the other hand. Slowly slide the stack splint onto the affected finger until it completely fits. Make sure to check that the stack splint fits completely and the finger is really straight. If the finger is slightly bent either forward or backwards, it can lead to the development of sores at the knuckle. If the stack splint has a built in adjustable strap, you can use that to secure it in place without taping.
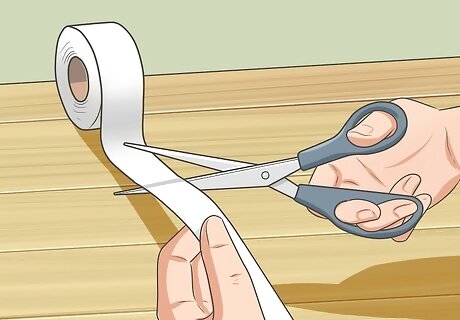
Use tape if necessary. Using scissors, cut a ten inch (25 cm) length of medical tape. Wrap it firmly around the finger and splint beyond the first knuckle. Some stack splints have built-in adjustable straps, so taping is not necessary.

Check the circulation of the trigger finger. For just a couple of seconds, pinch the nail of your trigger finger. This will cut off the blood flow and turn it white. Then let go. If the nail becomes pink within one to two seconds, then it has good blood circulation and your splint is on correctly. If it takes more than two seconds for the blood to return to the area, your splint is on too tight. Your finger needs adequate blood flow to heal. Remove and reapply the splint, adjusting for tightness.

Keep the splint on for four to six weeks. Unfortunately, the average trigger finger takes this long to heal. In mild cases, it may heal in only two to three weeks time; however, it greatly depends on the injury and the extent and severity of the inflammation in the affected trigger finger. Because they only immobilize the top of your finger, stack splints are somewhat less obtrusive than other splints. It may therefore be more possible to keep them on at all times without major inconvenience. This is likely the best option for proper healing, but consult with your doctor. Immobilization is imperative. In order for your finger to heal, try to keep from using it as much as possible. Replace/re-position the splint (and tape) when they become dirty, the tape starts to peel up, or if it becomes too loose to be effective. Visit your doctor after four to six weeks (or as previously advised) if your finger hasn't healed. He or she will be able to give you the proper management skills to take care of your injured trigger finger.
Understanding Dynamic Splints

Talk to your doctor about dynamic splints. Dynamic splints are the most complicated of all finger splints, because they are often spring-loaded and always custom fitted. This means that they are not universal and require further assessment by the physician first. To splint your trigger finger with this method, you'll need to see your doctor. Unlike other splints, dynamic splints use tension to actively engage the flexing and positioning of the injured finger. They are, in a matter of speaking, on-hand physical therapy. Dynamic splints are only worn during rest or periods of inactivity, usually for just a few hours at a time. This allows for correct positioning of the muscles, ligaments, and tendons, which need to be in a relaxed state.

Have your splint fitted and applied. Once your doctor recommends a dynamic splint and selects the proper type and fit, he or she will apply it. Here's what will happen: The physician will advise you to straighten the affected finger while supporting it with the other hand. Some situations require the finger to be slightly bent depending on the position to be corrected. The physician will now fit the dynamic splint onto your trigger finger until it completely fits. Further assessment will be made by the physician to correct positioning, alignment and proper fit. He/she will also check the pulse to see if the site has good circulation. He/she will instruct you to bend the affected finger. It should return back to a straight position because of the spring attached to the dynamic splint.

Schedule follow-ups. Proper instruction will be given by the physician regarding how long the dynamic splint needs to be used. Once everything is completed, schedule a follow-up check-up in order to assess improvement of your injured trigger finger. If you experience any complications, such as poor circulation, unusual pain in the digit, numbness, or tingling, or the splint doesn't seem to be effective, visit your doctor before your scheduled follow-up. It will likely just require a quick realignment of the splint.

















Comments
0 comment