views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
Running, walking, and jumping may be especially painful, an upsetting experience if you are an athlete, or even just a weekly walker. Anyone can develop stress fractures, from sedentary people to Olympic athletes. Studies show that by being aware of the risk factors, understanding the symptoms, and getting a professional diagnosis, you can identify and confirm the source of your injury.[2]
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
Recognizing Common Symptoms
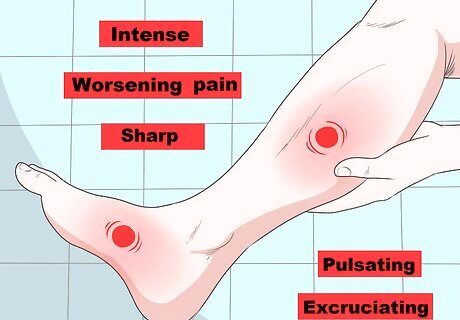
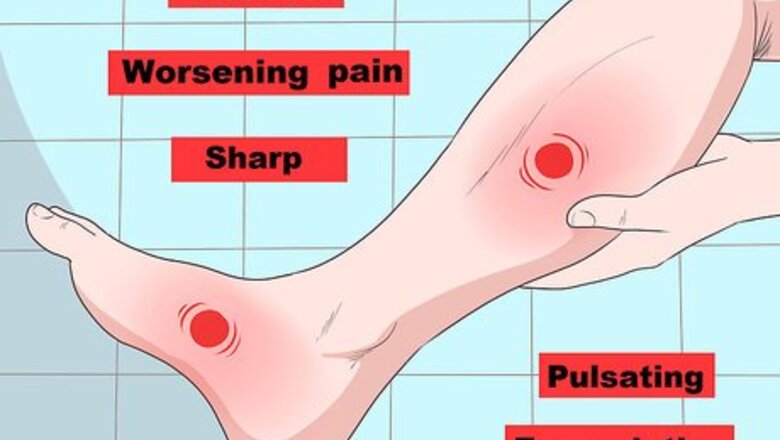
Take notice of an intense or worsening pain. Pain in the affected area is the most common symptom of stress fracture, especially pain that intensifies with activity. Although pain from a stress fracture can be barely noticeable at first, it may become worse over time. The pain may be sharp, pulsating and excruciating.

Keep an eye out for inflammation, swelling, or bruising. If inflammation, swelling, or bruising are present at the site of pain, this indicates the possibility of a stress fracture. Some areas where you might notice inflammation, swelling, or bruising include: On the top of your foot. Along your shin (the front of your calf). Around your ankle or heel.

Notice the presence of localized tenderness. Localized tenderness usually originates from a specific spot and decreases during rest. Tenderness or the feeling of a palpitating soft object can be due to inflammation in the affected area. Touch the affected area to see if it is tender.

Note any muscle spasms. When the muscle fibers in the injured area stretch or tear due to a stress fracture, they contract. This contraction may lead to muscle spasms and more pain in the affected area. You may notice that the area feels tight, cramped, or achy.
Evaluating Your Risk Factors
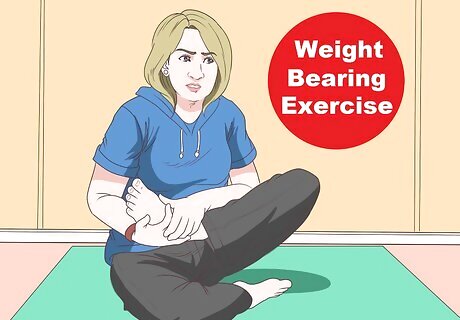
Monitor any weight-bearing exercise or activities with repetitive motions. Stress fractures are caused by putting too much weight or pressure on the weight-bearing bones of the body, like those in the legs and feet. This weight can cause an imbalance in the growth of new bone cells. Constant overuse of weight-bearing bones can lead to bone exhaustion, which can crack the bone and lead to a stress fracture. Low-impact exercises, like yoga, can also cause stress fractures if they use too much repetitive motion. These fractures are more likely to appear in the feet. Stress fractures usually occur in the tibia (shin bone), fibula (lower leg bones), metatarsals (bones of the feet), and navicular (mid-foot bone). They occur less often in the hip bones, pelvis, and sacrum.
Consider a recent increase in activity. People who increase their physical activity after being sedentary for a long time have a higher likelihood of developing stress fractures. This can come as a shock and be the first sign of overtraining. If you have just upped your running mileage dramatically or recently started a new workout regimen, then you may be suffering from a stress fracture.
Know that athletes are at a heightened risk of stress fractures. Many sports, such as track and field, basketball, tennis, and gymnastics, cause repetitive stress on the bones. This stress is due to the foot striking the ground, causing trauma that can lead to stress fractures. Athletes who overtrain on different surfaces and those who use substandard equipment, like worn out athletic shoes, are at an increased risk of stress fractures.
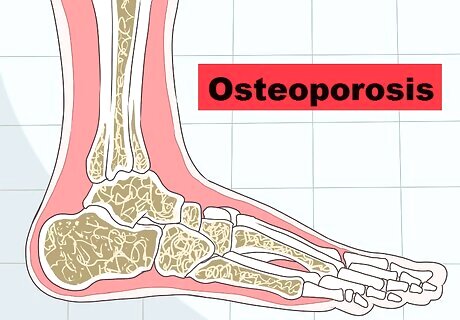
Identify preexisting medical conditions that heighten your risk. People with preexisting medical conditions, especially osteoporosis, are prone to developing stress fractures because they have weak and brittle bones. Osteoporosis is a condition that weakens bones and may lead to stress fractures.
Track your use of corticosteroids. Corticosteroids provide relief for conditions like arthritis, skin rashes, and asthma. Corticosteroids can, however, increase your risk of getting a fracture, especially if you have been using them for a long time. When getting your injury examined, be sure to tell your doctor if you are using corticosteroids.
Be aware that women are more prone to stress fractures. Women, especially those who exercise and diet to an extreme degree, have irregular periods, and/or have osteoporosis, are at an increased risk of stress fractures. This is known as the female athlete triad and it leads to brittle bones that are likely to break easily.
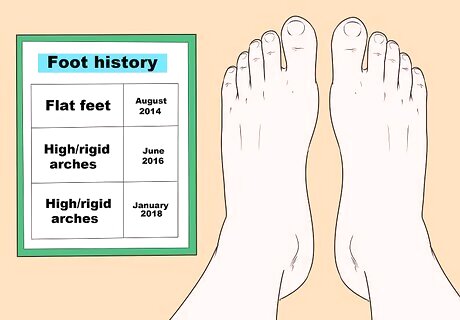
Reflect on any history of foot problems. Individuals with foot problems, like flat feet or high and rigid arches, are prone to developing stress fractures. This is due to the imbalance these foot abnormalities cause during weight-bearing activities. If you have a history of foot problems, then it is more likely that you will experience a stress fracture.

Consider lifestyle factors that increase your risk of stress fractures. People who drink more than 10 alcoholic drinks per week or smoke are at a higher risk of developing stress fractures. This is because substances in alcohol and cigarettes tend to reduce bone density. Additionally, people with eating disorders have reduced amounts of calcium and vitamin D, which are both necessary nutrients for strengthening the bones.
Getting a Professional Diagnosis
See your doctor. Check with your doctor or a specialist, like a podiatrist or an orthopedic surgeon, if you experience pain while doing weight-bearing exercises such as walking, running, and jogging. Remember that in the case of a stress fracture, the pain usually subsides at rest. When the pain, discomfort, and swelling do not subside, it is best to head to the emergency department of the nearest hospital or treatment facility. If left untreated for too long, a stress fracture can cause quite a bit of damage.
Discuss your medical history. The doctor will interview you and ask you some questions to gather information. This information will aid the doctor in accurately diagnosing a stress fracture. The doctor can also evaluate your risk factors for developing a stress fracture with this information.
Get a physical examination. During a physical examination, a doctor will inspect, palpate, and percuss the affected area. This may be enough for the doctor to make a diagnosis because symptoms such as tenderness, pain, and swelling can be detected in this manner.
Get an X-ray. An X-ray may not show evidence of stress fractures, but it can be used to detect signs of a stress fracture several weeks after the symptoms begin. These signs can show when the bone starts to remodel and heal at the fracture site. In this case, an X-ray may help the doctor confirm the diagnosis. Since stress fractures might only appear as a crack in the bone, their extent and severity may not be visible in a routine X-ray. If the X-ray is unsuccessful, further imaging may be necessary.
Ask about a computed tomography scan. Computed tomography (CT) scans take computerized images and convert them to provide a clearer picture of the affected site and its surrounding joints, ligaments, and bones. This may help to detect a stress fracture if an X-ray does not identify the problem.

Go for a bone scan. A bone scan uses a radioactive tracer injected through an intravenous line to demonstrate areas where bone cells have increased activity and blood supply. These areas indicate that there has been bone repair with a bright white spot on the scan image. However, a stress fracture may look the same as another type of bone injury on a bone scan, so it is not the most accurate imaging test for identifying stress fractures.

Ask about magnetic resonance imaging (MRI). An MRI uses radio and magnetic field waves to form a more detailed and clear picture of the scanned body structure. Try to have an MRI within the first week of the injury to identify a stress fracture. This will provide the most accurate results and can distinguish between a stress fracture and a soft tissue injury.

Talk to your doctor about treatment options. In most cases, all you need to do is rest and stop any vigorous activities until your injuries heal. If your injury hasn't healed in 6-8 weeks, your doctor may recommend surgery to insert screws into the foot. You may need to wear special footwear for a few weeks after this surgery. It is a good idea to stop the activity that caused your stress fracture for 6-8 weeks after your injury. Ask your doctor if calcium or vitamin D supplements can help you as you heal.


















Comments
0 comment